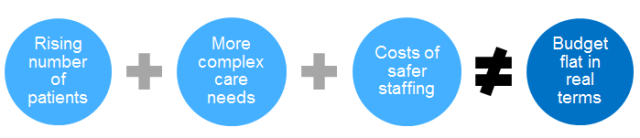
Our last blog described how the proposed 2015/16 national tariff aims to help the health sector bridge the gap between growing cost pressures on the NHS and a flat budget in real terms.
To develop our proposals, we relied heavily on the knowledge and expertise of people in the healthcare sector.
This blog explains how we engaged with the sector and what we heard.
Supporting parity of esteem between mental and physical health services
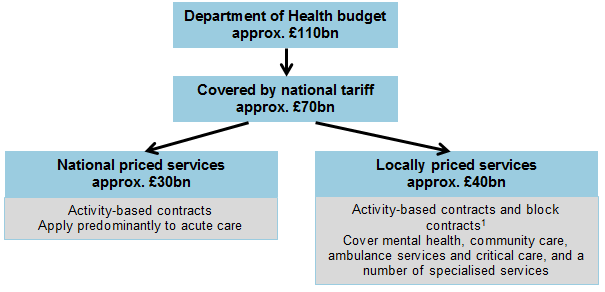
Monitor is strongly committed to supporting parity of esteem between mental and physical health services, and is not recommending cutting budgets for any services. In fact, expenditure on mental health services across the NHS- trusts, primary care, community and specialised services -is in fact actually going up for 2014/15 in real terms.
Furthermore, under the NHS payment system, national prices are not set for mental health services. Pricing decisions for mental health services are made at local level by commissioners and providers, who are expected to have regard to the national rules but can make their own price adjustments where there are good reasons to do so.
Developing the 2015/16 national tariff
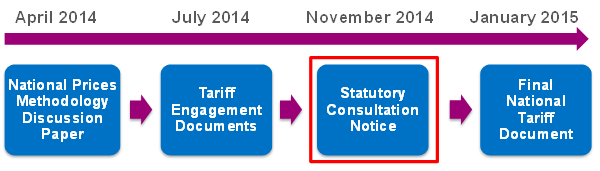
We decided to develop the 2015/16 national tariff gradually in four stages (see chart below), so we could seek input from the sector at each stage and incorporate it in the next one. This way stakeholders can see how their views are reflected as the process advances.
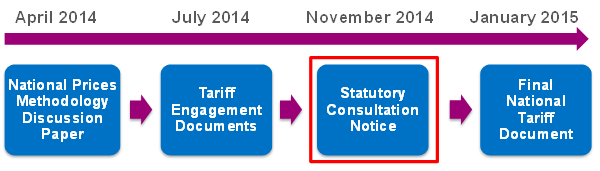
We decided to develop the 2015/16 national tariff gradually in 4 stages.
In the first stage, we explained the decisions we had to make in the 2015/16 national tariff in a discussion paper. The paper sought early views on some of the key issues, and called for evidence on matters that were important to stakeholders.
In the second stage, we asked for people’s views on a comprehensive list of proposed changes to the national tariff for 2015/16 and the reasons behind them, published as a set of Tariff Engagement Documents.
The next stage, currently underway, is a statutory consultation on what we propose to put into the 2015/16 national tariff in as close to final form as possible.
Monitor is required to publish these proposals as a statutory consultation notice under Section 118 of the Health and Social Care Act 2012. The 2015/16 notice, published on 26 November, includes those parts of last year’s tariff that we intend to leave as they are well as all the changes we propose for 2015/16.
This consultation includes a statutory process enabling relevant providers –foundation trusts, licensed independent providers and other providers of NHS services for which there is a national price – and clinical commissioning groups to object formally to our proposed method for calculating national prices.
If 51% or more relevant providers or 51% or more clinical commissioning groups object, we may need to refer to the Competition and Markets Authority before publishing the final national tariff (the fourth and last stage). But we hope that having engaged with providers and commissioners throughout the year and addressed their concerns where there was enough evidence, we can reach a satisfactory level of understanding and agreement. If that proves to be the case, and having considered all the other responses to the consultation, we would expect to issue the final national tariff document for 2015/16 in the New Year.
Engaging with stakeholders
Publication at each stage was preceded by targeted engagement (for example, to seek clinicians’ views on draft national prices) and followed by a wider set of opportunities for stakeholders to share their views with representatives from Monitor and NHS England.
- we held a number of workshops in Birmingham, Leeds and London. The majority covered the range of proposals for the tariff (see a summary of the discussions), but we also held a couple of workshops specifically on mental health (see a summary of one of these workshops)
- we ran 4 webinars, which discussed the proposals at varying levels of detail: watch them again
- we have also used our mailing lists, Twitter and LinkedIn to get the message out to as many people as possible
The national tariff is a technical document and the development process and final document tend to appeal to a narrow audience. So while we sought the views of patients and their representatives, much of our actual engagement was with other parties representing different perspectives on patients’ interests, in particular:
- clinical commissioning groups, who buy the care their local population requires
- providers (such as hospitals), who know how much it costs to deliver care
- clinicians and carers (and their representatives, such as the Royal Colleges), who work with patients to deliver the most effective, safe and patient-focused care
What stakeholders have said
We have received a lot of useful feedback so far. Stakeholders have told us they appreciate the efforts we have taken to make the process of setting the national tariff more transparent. But some have raised concerns about the length of documents and use of technical terminology. We are addressing these concerns by trying to make our communications more accessible and easier to understand.
Some feedback also highlighted a difficult conundrum: the national tariff needs to change quickly and fundamentally in order to enable new patterns of care, but mandating these changes without first testing them could destabilise the system. In response, we are looking to work with a selection of test sites to trial a number of innovative payment approaches that could support new models of care. Lessons from these trials will inform any wider roll-out of new payment approaches in future.
Most of the specific proposals we have made for 2015/16 over the past year have been received positively. For example, there has been widespread support for introducing a ‘best practice tariff’ that would incentivise better care for heart failure patients, and for clarifying what is required to improve the transparency of contracts for mental health services.
We have, of course, also considered stakeholders’ objections to our proposals. For example, stakeholders were largely sceptical about the benefits of using data on activities and costs from multiple years to set national prices. We took this feedback on board and have decided to stick to using data from one recent year only.
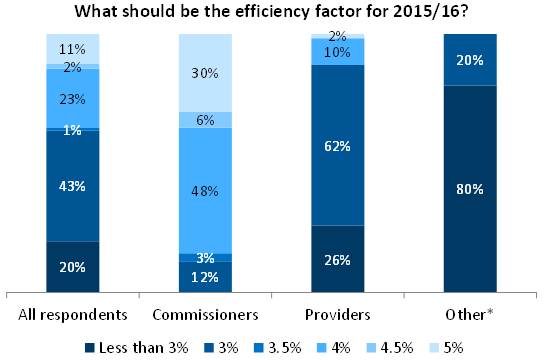
The policy that generated the most interest and debate was probably the ‘efficiency factor’. This is the percentage by which prices in the national tariff are reduced to reflect the amount providers can be expected to save by becoming more efficient while still maintaining or improving the quality of care they provide.
The efficiency factor has been set at 4% in recent years. Many providers told us that they are running out of opportunities to make further savings. They generally advocated for an efficiency factor of 3% or lower for 2015/16.
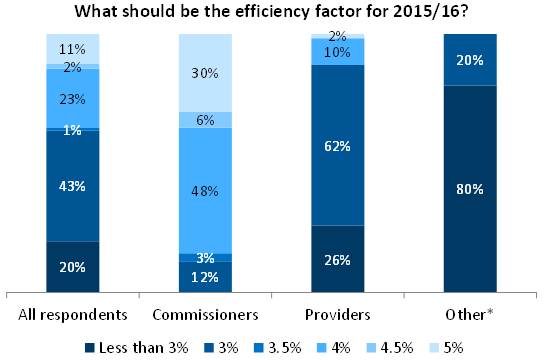
A summary of stakeholder views on the efficiency factor.
* ‘Other’ includes clinicians and suppliers of drugs and medical devices
Commissioners, on the other hand, offered a wider range of views. The majority were concerned they might not be able to afford all the care that their population would require unless prices fell materially. They sought an efficiency factor of 4% or higher. But some commissioners were more concerned by the financial implications for providers of asking them to deliver 4% efficiencies for another year. These commissioners suggested that an efficiency factor of 3 to 3.5% was more appropriate.
We have taken the range of views on board in proposing an efficiency factor of 3.8% for the 2015/16 national tariff in the statutory consultation notice.